HAVING radioactive seeds implanted in the prostate to treat cancer is just as effective as major surgery to have the whole prostate removed, according to a new study.
The treatment, called brachytherapy, involves having tiny implants – each one little bigger than a grain of rice – inserted close to the tumour site.
Once in place, the seeds gradually emit radiation to slow or stop cancer growth, while causing little ‘collateral’ damage to surrounding healthy tissue, as can happen with external beam radiotherapy – where the radiation is beamed through the skin, passing through healthy tissue on the way.
Within a year the seeds will have released the vast majority of their radiation – and they can then be safely left in place for good without doing any harm.
The treatment is sometimes seen by patients as a more palatable alternative to a radical prostatectomy – surgical removal of the entire prostate – which can cause urinary incontinence and erectile dysfunction.
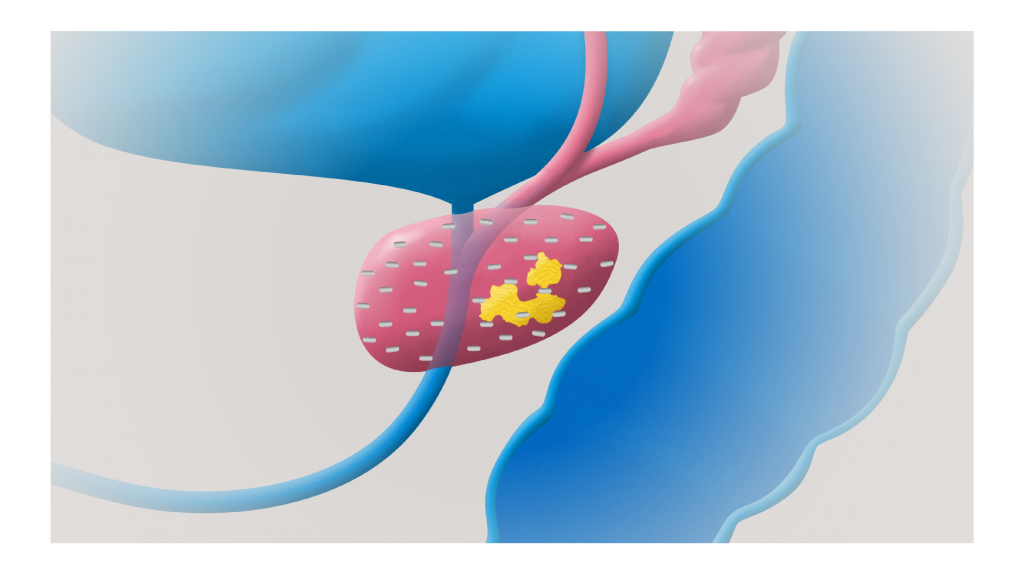
Implanted bracha seeds
But there have been long-running doubts about whether brachytherapy can match surgery in terms of ‘curing’ cancer and improving survival rates.
Doctors at a group of universities and hospitals in Japan compared long-term outcomes in 933 men who were treated with brachytherapy and 334 who underwent a radical prostatectomy.
In all cases the men’s cancer was said to be of ‘intermediate risk’ – in other words it hadn’t spread beyond the prostate.
The researchers tracked recurrence rates of cancer among the men by monitoring changes in levels of their prostate specific antigen – a protein in the blood which can indicate cancerous growth when levels are raised.
The results, published in the journal Radiation Oncology, revealed that eight years after treatment, survival rates between the two groups were very similar – 76 per cent in the brachytherapy patients and 74 per cent in the surgery group.
Findings were also very similar in terms of being cancer-free after eight years – 98.5 per cent in the brachytherapy men versus 99 per cent in the surgical group.
In a report on the results, the researchers said: ‘There was no significant difference between patients treated with brachytherapy seeds and those treated with radical prostatectomy.’
Professor Langley’s comment:
For Intermediate risk disease Brachytherapy is a viable option and may have less risk of impotence and incontinence. There is however still a very small risk of radiation injury to surrounding tissues. Other studies comparing radiation treatments and surgery using similar statistical techniques has also shown equal efficacy. Our advice is that patients should consult both a surgeon and a radiation oncologist before deciding what treatment works best for their individual circumstances.




